Healthcare Hero Turned Data-Driven Consultant: Q&A with Mary Jagim

For more than 25 years, Mary Jagim, RN, MSN, CEN, FAEN, has been a nurse. Once a nurse always a nurse, am I right!? While Mary may no longer be at the bedside, she continues to pursue her passion for working in healthcare and providing the absolute best care for patients. With the continued rise in staff violence, we knew we had to discuss her career and her opinions on how healthcare leadership can support staff, ensuring they feel safe and valued while doing the job they love.
When speaking to Mary, her passion shines through. She is committed to helping healthcare organizations support current and future clinical staff so they can have long, fulfilling, and successful careers.
Read on to learn more about Mary, her insights on the healthcare industry, her experience as an Emergency nurse, and the current landscape in healthcare technology.
Q: Mary, tell us about your background and how long you have been a nurse.
You can say I’ve worked in healthcare my entire life. My mother was the assistant director of nursing at a local nursing home, and when I was 12 years old the director of nursing offered me a position there. My after-school job was to help bring the residents down to the dining hall and back up to their rooms after mealtime. At 16, I worked as a nursing assistant during the summers. This experience led me to pursue a career in nursing. Upon graduation, I worked in the emergency department first in Duluth, MN and then in Fargo at what was then MeritCare, where I stayed for more than 20 years.
Q: Why the emergency department (ED)?
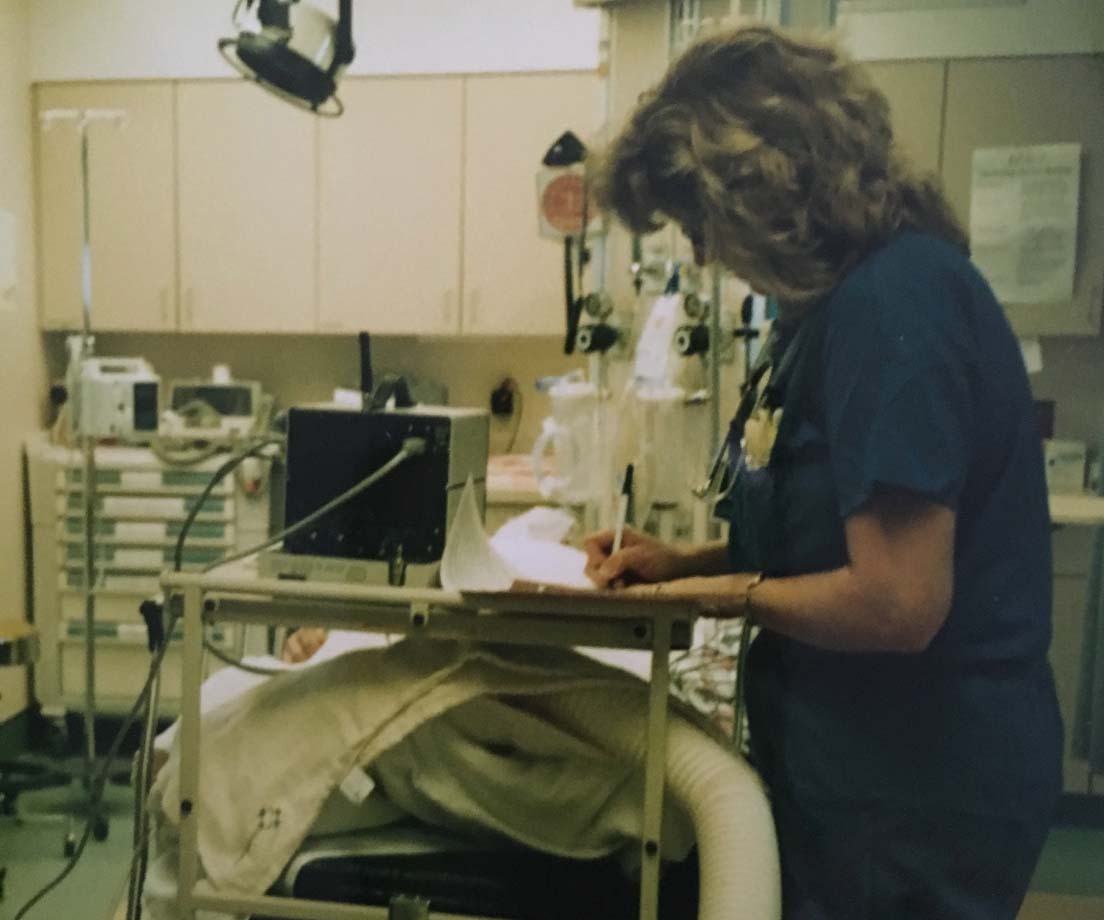
Fun fact, I worked as a scrub nurse during nursing school and helped to deliver almost 100 babies! I chose the ED because I was attracted to the change of pace and the variety. That is what always intrigued me. In the ED, you took care of everything from newborn babies to the elderly – minor cuts and scrapes to major traumas. You never knew what was going to come through the door next. Many of my former colleagues and I were drawn to that variety in who you care for. You could have 3-4 patients at one time with completely different cases.
The adrenaline rush of the ED truly kept me going all of those years. I also had incredible mentors when I was a new nursing school graduate. I get teary-eyed thinking about my mentors because they really made me an emergency nurse. They showed me how to handle something when I felt like I didn’t know how. I really credit them because those first three years or so are so critically important. They taught me everything I know about being an emergency nurse. I can’t imagine working in another specialty or department.
Q: Was there safety training back then to teach you and other staff how to keep yourselves safe in case of emergency?
A: I learned so much while I was still in nursing school. I deliberately chose to work nights because I thought that would be the most interesting and challenging experience. During my rotation at Regions Hospital in the ED, I learned a lot from the staff and law enforcement who provided security in the department on how to keep myself safe. During the time I was an ED manager, we started to receive more formalized training.
Now, in a lot of the hospitals and IDNs I work with and across the country, there are defined training programs – how to de-escalate conflict, and how to understand the way to keep yourself safe in a situation. Staff are taught to call for help, if needed, how to deflect, contain and control a situation until they can get more resources. So much has changed since I was at the bedside, but some things have stayed true. The importance of ensuring staff are well-prepared in case of emergencies, knowing the steps to take when additional help is needed and ensuring adequate security resources to support staff.
Q: In your opinion, why does workplace violence occur and what can healthcare administrators do to support staff?
A: Hospitals, and especially emergency departments, face a unique challenge of needing to “be there” 24/7 and open to the community while also trying to protect patients and staff from threats within the community. Hospitals are a place of high emotions as well as a place where individuals with drug and alcohol issues, as well as mental health concerns are seeking care. It’s sometimes very difficult to anticipate incidents of violence. Workplace violence is not new and has gotten progressively worse, especially in the healthcare industry. When I was Government Affairs Chair of the North Dakota Emergency Nurses Association (ENA) in 1995, I helped get legislation passed in the state legislation that made it a felony to assault emergency department staff. For the last 20 years, organizations such as the Emergency Nurses Association (ENA), American College of Emergency Physicians (ACEP) and the American Nurses Association (ANA) have been advocating for felony assault laws and well as stricter workplace safety regulations. In recent years, The Joint Commission has issues enhanced standards focused specifically on workplace violence. All of these initiatives are helping to enhance the supportive foundation for a safer work environment.
Q: Can you talk about how the use of RTLS (Real-Time Location System) can help decrease workplace violence?
A: Real-Time Location Systems and staff duress solutions are making a difference in hospitals. First, it gives nurses and hospital staff a tool to call for help. It is physically located on them in the form of a wireless staff badge. When I worked in the ED, we had panic buttons on the wall, but nothing physically worn by the staff to allow them to call for help from wherever they are. Patients can make unexpected movements – visitors too – that cannot be anticipated. When staff are in a situation where they feel unsafe, they need to be able to call for additional resources – wherever they are located. Sometimes, it can be a situation where they must call for help without bringing attention to themselves. This is where wireless call functionality is crucial.
Second, as a consultant for CenTrak, I am always talking about data. Data is my middle name! Our safety solution provides an abundance of data for clinicians, hospital staff and administrators. When a staff member summons help via the staff badge, the ‘press’ is reported. Even if the press does not result in a violent event, our reporting will show that the staff member felt a need to press. This is critically important to help understand the risk and develop strategies to mitigate.
In addition to staff duress solutions and data generated by RTLS, large health systems that we work with have workplace violence committees in place. Some have even created specific roles at the executive level to determine, understand and navigate the prioritization and deployment of various staff duress solutions. These roles typically bridge the gap between staff (both clinical and non-clinical) and the hospital or health system’s decision-makers.
Q: How can staff have an open dialogue with administrators and bring workplace violence-related issues to the forefront?
A: When meeting with customers on–site, we gather data from staff in the form of staff surveys on their comfort level – how safe do you feel? This helps administrators understand what is happening in their facilities and on the floor. It reminds me of Maslow’s hierarchy of needs - "a pyramid describing several levels of the human experience, that allow an individual to feel fulfilled.” Safety and security, being near the base of the hierarchy represents a foundational need for all humans. If administrators do not create a safe environment, there will continue to be turnover, low job satisfaction, and staff shortages in the healthcare industry.
Something else I’ve seen at customer sites and across the healthcare industry is a desire for continued communication between leadership and clinical staff. Those prioritizing staff safety have adopted best practices such as:
- Creating steering committees to allow for open dialogue whereby staff can raise concerns with upper management and hospital leadership.
- Adding a new, dedicated staff member whose sole purpose is to address workplace violence issues and foster a safe working environment for all.
- Engage staff at all levels of the organization in developing safety strategies.
Q: How has your role as a nurse (in the emergency department) helped you as a consultant at CenTrak?
A: My experience as an emergency nurse and nurse leader has helped immensely with my role as a consultant. Understanding hospital operations is key to successfully implementing RTLS technology so that it can best support the patient and staff experience. Having experienced workplace violence myself, I understand the urgent need to provide effective solutions to help staff get assistance when being threatened. As an emergency department manager, the number one thing that kept me awake at night was my fear that one of my staff would be assaulted. And during my term as president of ENA in 2001, I heard many stories from nurses who had been assaulted and who did not feel their organization supported them.
The rise in violence since the COVID-19 pandemic has only escalated the need to address the issue of workplace violence. The bottom line? Staff need to feel safe at work if they are going to be able to provide good care for their patients. That means support from the top down of their organization, enterprise-wide workplace safety initiatives, and staff engagement in order to have a solution that gives staff a sense of safety and support.






